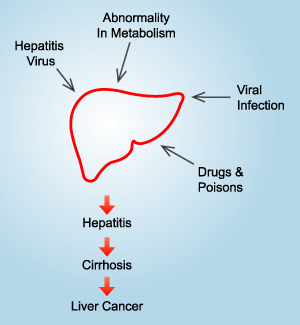
LIVER DISEASES
Liver diseases is a worldwide problem. Conventional drugs used
in the treatment of liver diseases are sometimes inadequate and
can have serious adverse effects. It is, therefore, necessary
to search for alternative drugs for the treatment of liver diseases
to replace currently used drugs of doubtful efficacy and safety.
Below are some liver diseases caused by toxic chemical and toxicological
problem.
1. Hepatitis B
(a.) What is Hepatitis
B?
Hepatitis B is a serious disease
caused by a virus that attacks the liver (Hepatitis B virus
- HBV). Infection with the HBV may be without any symptoms,
mild or severe. Over time, hepatitis B can destroy the liver
(cirrhosis) and can cause hepatocellular carcinoma (liver
cancer).
|
|
(b.) What is the risk of Hepatitis B?
- It has been estimated there are approximately 350
million HBV carriers in the world, of whom 80%
are Asians.
- HBV is reported to be 100 times more infectious
than HIV.
- People who are at higher risk, including people who live with
hepatitis B carrier or patient. In acute hepatitis, it may takes
1 to 6 months from the time of infection until the disease manifests
itself.
- About 1% of patients infected with hepatitis
B die due to liver damage in this early stage.
- Carriers of HBV are 200 times more likely
to develop liver cancer decades after initial infection.
- The risk of becoming chronically infected depends on the age
at the time of infection. More than 90% of newborns, about 50%
of children, and less than 5% of adults infected with hepatitis
B develop chronic hepatitis.
(c.) What causes Hepatitis B?
HBV is spread by direct contact with
blood or other body fluids of infected people.
HBV is most commonly transmitted
by:
- sharing drug needles
- engaging in high-risk sexual behavior (especially anal sex)
- from a mother to her baby during childbirth and in the health-care
setting
(d.) What are the signs and symptoms of Hepatitis
B?
Early symptoms may include nausea and vomiting,
loss of appetite, fatigue, and muscle and joint aches. Jaundice,
together with dark urine and light stools, follows.
- Fatigue, malaise, joint aches, and low-grade fever
- Nausea, vomiting, loss of appetite, and abdominal pain
- Jaundice and dark urine due to increased bilirubin
(e.) How is Hepatitis B treated?
Acute hepatitis
- needs no treatment other than careful monitoring of liver function,
by measuring serum transaminases and prothrombin time.
Liver failure
- the patient should be monitored in an intensive care unit. Because
liver damage decreases the liver's ability to degrade proteins,
the patient's protein intake should be restricted. Patients should
be monitored until they recover or until a liver transplant appears
necessary. A liver transplant is the only definitive cure in cases
of liver failure.
Chronic hepatitis
- is geared towards reducing inflammation, symptoms, and infectivity.
Treatment options include interferon (administered by injection)
as well as lamivudine and adefovir dipivoxil (administered orally).
Liver transplantation is used to treat end-stage chronic hepatitis
B liver disease.
Go to top
(a.) What is alcoholic hepatitis?
Alcoholic hepatitis is an inflammation
of the liver that lasts one to two weeks. Symptoms include
loss of appetite, nausea, vomiting, abdominal pain and tenderness,
fever, jaundice, and sometimes, mental confusion. It is
believed to lead to alcoholic cirrhosis over a period of
years. Cirrhosis involves permanent damage to the liver
cells. "Fatty liver" is the earliest stage of
alcoholic liver disease.
|
 |
(b.) What is the risk of alcoholic hepatitis?
Long-term alcohol abuse is may cause cirrhosis and eventually
liver cancer. It may be fatal, especially if the patient has
had previous liver damage. Those who have had nutritional deficiencies
because of heavy drinking may have other ailments. These medical
complications may affect almost every system in the body. It
is important to recognize and treat alcoholic cirrhosis early,
so that these life-threatening consequences are prevented.
(c.) How is alcoholic hepatitis diagnosed?
Alcoholic hepatitis is not easy to diagnose. Sometimes symptoms
are worse for a time after drinking has stopped than they were
during the drinking episode. While the disease usually comes
on after a period of fairly heavy drinking, it may also be seen
in people who are moderate drinkers. Blood tests may help in
diagnosis. Proof is established best by liver biopsy. This involves
taking a tiny specimen of liver tissue with a needle and examining
it under a microscope. The biopsy is usually done under local
anesthesia.
(d.) How can alcoholic hepatitis be treated?
The best treatment is to stop drinking. Treatment may also
include prescribed medication, good nutrition, and rest. The
patient may be instructed to avoid various drugs and chemicals.
Since the liver has considerable ability to heal and regenerate,
the prognosis for a patient with alcoholic hepatitis is very
hopeful - if he or she totally abstains from drinking alcohol.
Patients may also take liver tonic such as Phyllanthus
to improve their liver functions.
Go to top
3. NASH (Nonalcoholic Steatohepatitis)
(a.) What is nonalcoholic steatohepatitis?
Nonalcoholic steatohepatitis (NASH) is described as inflammation
of the liver associated with the accumulation of fat in the liver.
NASH is not connected with other causes of chronic liver disease,
including hepatitis B and C viruses, autoimmune disorders, alcohol,
drug toxicity, and the accumulation of copper (Wilson’s
Disease) or iron (hemochromatosis).
(b.) What causes NASH?
There is no known specific cause of NASH. Men and women, overweight
or not, has diabetes mellitus or not, and did or did not have
excess lipids (fat) in their blood may suffer from NASH.
(c.) What is the risk of NASH?
In NASH, which resembles alcoholic steatohepatitis,
the inflammation of the liver is associated with an increase of
fat deposits and typically occurs in middle-aged, overweight,
and often diabetic patients who do not drink alcohol. It has also
been connected with rapid weight loss, or in women taking hormones
(estrogen). The fatty tissue in the liver may break up liver cells
(steatonecrosis) and the patient may develop cirrhosis (scarring
of the liver). Recent studies indicate that NASH can result in
the development of fibrous tissue in the liver (fibrosis) in up
to 40% of patients or cirrhosis in 5-10% of patients. Studies
report that the progression to fibrosis or cirrhosis for NASH
patients is variable but can occasionally occur in less that 20
years. Some studies have shown that 20% to 40% of people who are
grossly overweight will develop NASH.
(d.) How is NASH diagnosed?
Many NASH patients are unaware of their conditions
because they do not exhibit any symptoms. In most cases, NASH
causes a slight increase during liver enzyme tests, as do other
forms of liver disease. Images of the liver are obtained by an
ultrasound test, a CT scan, or an MRI scan. The diagnosis must
be confirmed by liver biopsy.
(e.) How is NASH treated?
Presently, there is no specific treatment for
NASH that is universally agreed upon. However, patients who are
obese, diabetic, and have high lipids (fats) in their blood are
advised to lose weight and control their diabetes and elevated
lipids. Usually, a low fat, low calorie diet is recommended along
with insulin or medications to lower blood sugar for diabetes.
For many patients with NASH whow are not overweight and not diabetic,
a low fat diet is recommended. Patients with NASH should avoid
alcohol or other substances that could be harmful to the liver.
Phyllanthus, a herb used traditionally
for liver ailments may be beneficial for patients with NASH.
Go to top
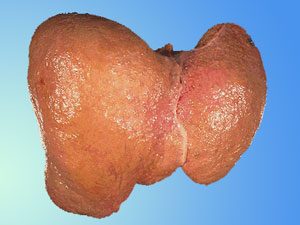
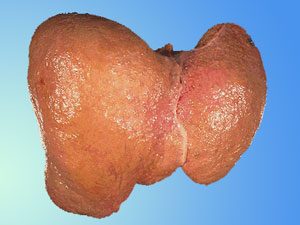
4. Cirrhosis
(a.) What is cirrhosis?
Cirrhosis is a term that refers to a consequence
of chronic liver diseases in which normal liver cells are
damaged and replaced by scar tissue, decreasing the amount
of normal liver tissue. The distortion of the normal liver
structure by the scar tissue interferes with the flow of
blood through the liver. It also handicaps the function
of the liver, which, with the loss of normal liver tissue,
leads to failure of the liver to perform some of its critically
important functions.
|
 |
(b.) What is the risk of cirrhosis?
Cirrhosis will lead to Hepatocellular carcinoma
(liver cancer) which represents more than 5% of all cancers in
the world, and the estimated number of cancer-related deaths exceeds
500,000 per year.
(c.) What causes cirrhosis?
There are a number of conditions that can lead to cirrhosis:
- Excessive intake of alcohol (most common)
- Chronic vial hepatitis, types B, C, and D
- Prolonged exposure to environmental toxins
- Some forms of heart disease (cardiac cirrhosis)
- Other factors.
(d.) What are the signs and symptoms of cirrhosis?
The onset of cirrhosis is often “silent”
with few specific symptoms to identify what is happening in the
liver. As continued scarring and destruction occur, the following
signs and symptoms may appear:
- Loss of appetite
- Nausea and vomiting
- Weight loss
- Enlargement of the liver
- Jaundice - yellow discoloration of the whites of the eyes
and skin occurs
- Itching - due to the retention of bile products in the skin
- Ascites - abdominal swelling due to an accumulation of fluid
- Vomiting of blood - frequently occurs from swollen, ruptured
varices (veins that burst) in the lower end of the
- Increased sensitivity to drugs - due to the inability of
the liver to inactivate them
- Encephalopathy (impending coma) - subtle mental changes advancing
to profound confusion and coma
- Many patients may have no symptoms and are found to have
cirrhosis by physical examination and laboratory tests, which
may have been performed in the course of treatment for unrelated
illnesses.
(e.) How is cirrhosis treated?
Treatment depends on the type and stage of the
cirrhosis. It aims to stop the progress of the cirrhosis, reverse
(to whatever extent possible) the damage that has already occurred,
and treat complications that are disabling or life-threatening.
Phyllanthus maybe helpful in
prolong the life span and improve the patient’s condition.
Go to top
|